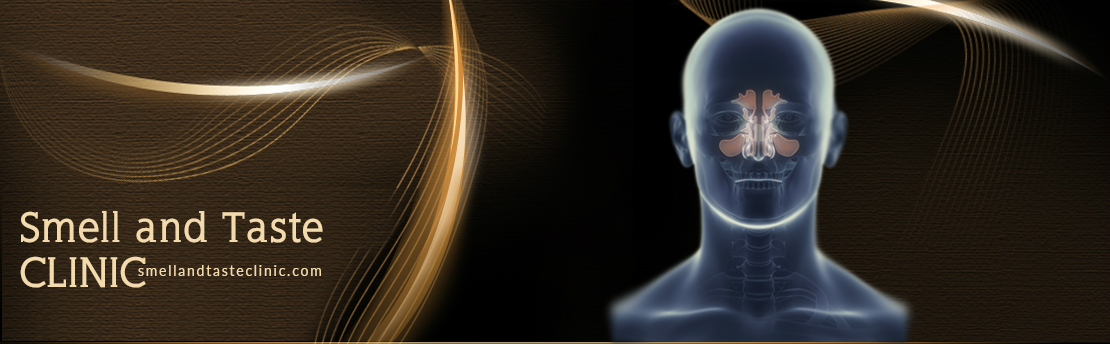
One of most common cause of smell loss is an ongoing process in the nose and/or sinuses, specifically rhinitis (inflammation in the nose), nasal polyps and/or sinusitis. The history usually is that of gradual loss of smell ability proceeding to total loss. Recurrent, rapid, temporary improvement in the ability to smell, often after exercise or showering, is often reported. Some patients report temporary improvement with medications, such as antibiotics or corticosteroids. True taste loss does not occur, but patients sometimes report the presence of foul tastes/smells. Other important features include difficulty breathing through the nose, post nasal drip, nasal allergies, and a history of sinusitis and/or nasal polyps. Chronic sinusitis may present with smell loss and no other chronic symptoms, however.
To evaluate a patient with loss of smell due to ongoing process in the nose and/or sinus, a physician performs an exam in the inside of the nose with nasal endoscopy. Endoscopy is a minimally invasive, diagnostic medical procedure consisting of a thin, rigid tube with fiberoptic cables for bringing in light source and a video camera to project magnified images on a screen. These endoscopic images are captured and recorded for documentation for each patient.
The nasal endoscopy allows a detailed examination of the nasal and sinus cavities of a patient with loss of smell in an outpatient clinic. It is currently the preferred initial method of evaluating smell problems that can be caused by nasal stuffiness and obstruction, sinusitis, nasal polyps, and nasal tumors. During the endoscopy, the patient is seated and the physician searches for areas of swelling in the mucosal membranes, presence of purulent secretions (pus) draining from the sinus openings, enlargement of the nasal turbinates (internal nasal structures that humidify the nose), crookedness of the nasal septum (the wall that separates the two sides of your nose); presence of polyps; sites of nasal bleeding; and the presence of tumors within the nasal and sinus cavities. If pus is observed, it may be sampled and cultured with a small swab to determine what organism is causing the infection.
Typically, nasal endoscopy is performed using the “three pass” technique, visualizing three main areas in the nasal and sinus cavities. In the first pass the nasal floor and the nasopharynx are viewed. The endoscope is then brought out and turned upwards and sideways in order to view the drainage areas of the nasal sinuses (middle and superior meati and the spheno-ethmoidal recess). In the third pass the endoscope is used to view the roof of the nose and the area of the olfactory cleft (smell region).
In order to make this procedure easier and minimize patient discomfort, just before nasal endoscopy the nose will be sprayed with: 1) a nasal decongestant, to gently reduce the swelling in the nasal membranes to permit an easy passage of the endoscope, and 2) a local anesthetic, which temporarily numbs the nose and helps to decrease the chances of sneezing from sensitivity. The procedure is rarely painful, but some patients may experience discomfort if the nasal cavity is unusually narrow or the nasal lining is very swollen. Additional numbing spray or a pediatric –sized endoscope may prevent such discomfort.
Overall, nasal endoscopy is a safe and low risk procedure. Nonetheless, potential complications such as mucosal trauma and bleeding may occur, particularly in susceptible patients with increased risk of bleeding, such as those receiving aspirin or other anticoagulant medications (i.e. Plavix, Coumadin, etc.). In addition, adverse reactions to the topical decongestants or anesthetic provided prior to the procedure may occur. Thus before administering these topical medications, patients’ allergies should be verified.